BioSocial Health J. 1(2):84-89.
doi: 10.34172/bshj.23
Systematic Review
Biosocial environmental faces of climate variability in health care: A systematic review
Fatemeh Zarei Conceptualization, Formal analysis, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, 1, * 
Ehsan Arzroomchilar Data curation, Investigation, Software, 2 
Author information:
1Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran
2Faculty of Theology, University of South Bohemia, České Budějovice, Czech Republic
Abstract
Introduction:
Human health is directly impacted by climate variations, leading to changes in weather patterns (e.g., heat waves, droughts, floods, storms), as well as indirectly affecting water, air, and food quality. This research aims to explore key strategies for addressing environmental risks resulting from climate variations in the healthcare sector.
Methods:
A systematic analytical approach was employed in this investigation, examining studies on climate change adaptation from 2022 to 2023. English publications were sought in renowned databases like Elsevier, PubMed, Web of Science, and Scopus. The search process consisted of two phases. Initially, articles focusing on climate change, climate variability, and global warming were identified using keywords like "Climate change," "Climate variability," and "Global warming." Subsequently, relevant articles were chosen for examination and analysis, using terms such as "Health," "Exposure," "Infectious disease," "Mental health," "Adaptation," and "Mitigation."
Results:
Primary healthcare systems are essential for enhancing resilience at both individual and community levels, acting as a critical framework for safeguarding global populations through accessible, cost-efficient, responsive, and dependable healthcare services. The evaluation of selected studies underscores the necessity of establishing resilient healthcare systems to counter climate change through adaptive or resilience-focused and mitigative strategies. Recommendations include bolstering the capacity of these systems, enhancing efficient and iterative risk management across all tiers, fostering collaboration across various sectors, formulating action plans, and making short- and long-term investments to enhance adaptability.
Conclusion:
Pivotal in safeguarding global populations, healthcare systems should prioritize the reinforcement of social resilience by implementing adaptive and mitigative measures in response to climate change.
Keywords: Climate change, Resilience, Health
Copyright and License Information
© 2024 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Climate change, defined by the United Nations Framework Convention on Climate Change (UNFCCC) as human-induced alterations in global atmosphere, is a major threat.1 Its effects include rising temperatures, altered precipitation, and sea level rise. The consequences are dire, with predictions of a 1.8-4 °C increase by 2100.2 Compared to a 1.5 °C increase, a 2-degree rise would lead to twice the water stress and a 70% rise in river flood victims.3 Similarly, species extinction rates would be 2-3 times higher.2 Climate change harms access to basic needs like water, food, and healthcare. It weakens social and environmental determinants of health like clean air and safe water,4 The Lancet called it the biggest health threat of the 21st century.5
Climate change also hurts economies, worsens inequality, and sparks conflict. It affects health directly through extreme weather and indirectly through water, air, and food quality. Heatwaves cause illness and death, while air pollution increases respiratory infections and heart disease. Infectious diseases like dengue fever and malaria are also worsened by climate change.6,7 Disasters take a mental health toll as well.8 The World Health Organization (WHO) predicts 5 million deaths due to climate change by 2050.9
Climate change significantly impacts tropical diseases, particularly neglected tropical diseases (NTDs). Their transmission patterns and prevalence are affected.10 Climate change alters factors like vector development rates and transmission dynamics.10 Health services are on the frontlines but are threatened by climate change. Rising sea levels, storms, and floods disrupt infrastructure and healthcare deliver.11 The health sector itself also contributes to greenhouse gases.4 Therefore, we must strengthen health systems to respond to the health impacts of climate change while also reducing their carbon footprint. In this research, the major strategies for dealing with environmental hazards resulting from climate change in the health sector are explained.
Materials and Methods
In this study, a systematic analysis approach was used to review studies on coping with climate change in the 2023-2024 timeframe. In this regard, English articles were searched in databases such as Elsevier, PubMed, Web of Science, and Scopus. The screening of articles was done in three stages. In the first stage, a combination of keywords “Climate change”, “Climate variability”, “Global warming”, and “Exposure to climate changes” were used to search for articles on climate change. In this stage, 60 articles were found, of which 6 articles were removed due to repetition and overlap of topics, thus 44 articles entered the second stage. In the second stage, using preliminary review, articles related to the impact of climate change on health were selected, and thus 21 articles entered the next stage. Finally, in the third stage, among the articles of the second stage, articles related to approaches to coping with climate change in the field of health were selected for study and analysis (n = 12), one article was removed due to lack of access to the full text, and eventually 11 articles entered the final evaluation stage. The process of selecting articles for systematic review used Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Figure 1). Then, the subject of the studies, the method used, and their results were examined and discussed in the findings section (Table 1).
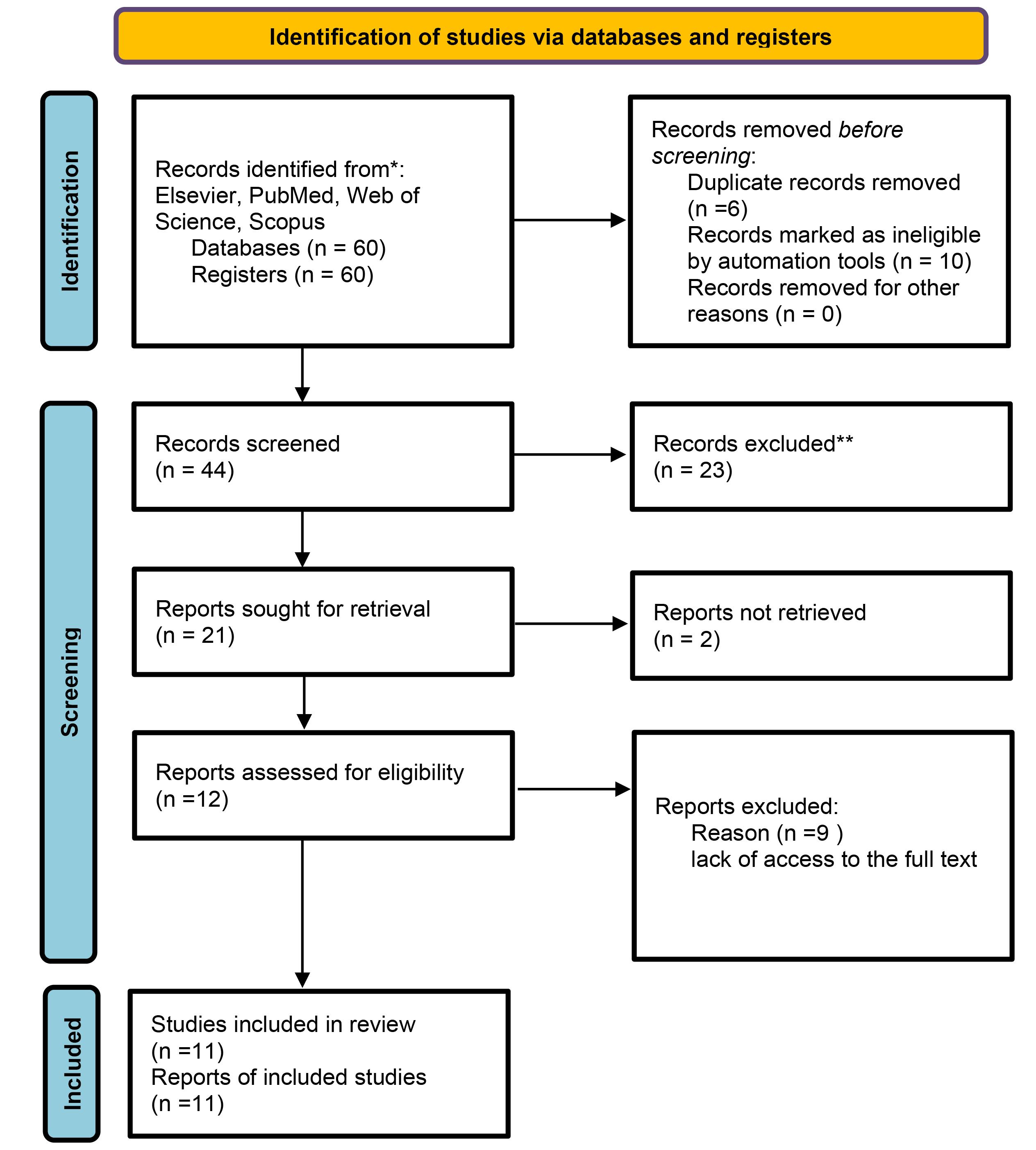
Figure 1.
Presentation of the process of selecting articles for systematic review using PRISMA diagram
.
Presentation of the process of selecting articles for systematic review using PRISMA diagram
Table 1.
Characteristics of reviewed articles on climate change-induced environmental health challenges
|
Author(s)
|
Topic
|
Methodology
|
Findings
|
| Li et al (2023)12 |
Impact of social vulnerability on health effects of climate change |
Systematic review |
Lack of theorization and indicator development that conceptualizes and operationalizes social vulnerability. |
| Thomson et al (2023)13 |
Designing a climate resilience maturity matrix |
Tool development |
Developed a climate resilience model that considers mitigation and adaptation approaches to enhance resilience. |
| Somani (2023)14 |
Global warming and its impacts on public health |
Analytical |
Pakistan, facing a persistent challenge of mitigating climate change impacts, requires urgent financial investment to build climate-resilient infrastructure and mechanisms to cope with the worst effects of global warming. |
| Conradt et al (2023)15 |
Assessment of the 2018–2019 European drought |
Remote sensing |
The event resulted in severe production losses in agriculture and forestry, while other economic sectors remained unaffected. However, there is no guarantee that this will continue to be the case if similar changes occur again. |
| Hartwell et al (2023)16 |
Examining barriers and facilitators to climate change action for public health agencies |
Survey: Online interviews |
Identified funding, state and agency-level prioritization, workforce capacity and capability, and political will as factors affecting preparedness for implementing climate and health activities. |
| Riva et al (2023)17 |
The association between energy poverty and mental health |
Cross-sectional analysis |
Exposure to energy poverty is associated with a significantly increased likelihood of poor general and mental health. Given the high proportion of Canadian households experiencing energy poverty, with established population health consequences, addressing energy poverty is imperative for equitable energy transition and climate resilience. |
| Scarr & Jagnoor (2023)18 |
Prioritizing climate change adaptation strategies |
Survey: Survey and priority ranking in global drowning prevention |
Prioritized criteria such as disaster risk reduction, sustainable development, child and adolescent health, and climate resilience over other criteria. |
| Kobayashi et al (2023)19 |
Genetic modification of agricultural crops to mitigate climate change |
Experimental study |
Increasing climate change threats such as methane-nitrous oxide emissions and global warming can be significantly mitigated using genetic modification of crops such as rice through improved water management technique. |
| Fehrer et al (2023)20 |
Analysis of climate change mitigation strategies in the health sector |
Qualitative study: Interviews with healthcare professionals |
Strategies refer to water and energy use, recycling and waste management, supply chain and procurement, digitalization, mobility, patient care, behavioral changes, and system level. |
| Rocklöv et al (2023)21 |
Decision-support tools for building climate resilience to emerging infectious diseases |
Systematic review |
Proposed innovative surveillance, prediction, testing, evaluation, and upgrading of surveillance and citizen science to increase preparedness and response to the growing threat of climate-sensitive infectious diseases. |
| Omri et al (2023)22 |
Climate-related health effects |
Analysis and description |
Urgent need for research and development towards reducing greenhouse gases due to negative impacts on public health, especially infants. |
Results
The impact of climate change on health systems
The escalating climate crisis significantly impacts health systems, as highlighted by Rocklov et al and Fehrer et al.20,21 Climate change’s effects on health are multifaceted, encompassing direct consequences like heat-related illnesses from extreme weather events, ecosystem disruptions affecting disease prevalence (waterborne, vector-borne), and social determinants like poverty and displacement that limit access to healthcare. Research by Thomson et al and Hartwel et al.13,16 further emphasizes how these pressures threaten healthcare access, service quality, and infrastructure stability, weakening health systems’ ability to respond effectively. As the climate changes, health systems must adapt to these immediate and future challenges to ensure continued service delivery.
The impact of meteorological events on health systems
Climate change disrupts health systems by hindering patient access to care and straining resources.23 Extreme weather events damage infrastructure, disrupt supply chains, and force displacement [e.g., forest fires]. These events also significantly impact mental health, both from the initial stress and the long recovery process.14,17 Energy poverty further exacerbates these issues, particularly for vulnerable populations.17 Climate-induced migration creates additional challenges, as refugees often lack access to healthcare, water, food, and shelter. Fear, language barriers, and unfamiliar healthcare systems further hinder their ability to seek help. Integrated programs are crucial to address these challenges by incorporating migrant needs into national and local health financing, policies, and interventions. Moreover, societies with higher existing mental health burdens are likely to experience more severe consequences from climate change.12
The impact of climate on the emergence of new diseases
Climate change fuels the emergence of new diseases in three ways: increased transmission of novel microbes, more viral diseases due to rising temperatures and precipitation changes, and the return of ancient viruses trapped in polar ice caps (e.g., malaria reaching mountains).24 These diseases, along with existing ones expanding their range (West Nile virus in Europe), worsen health problems in vulnerable groups (urban heat islands, pregnant women).25,26 Air pollution further exacerbates these issues, increasing respiratory and cardiovascular diseases.27 The combined effects strain health systems, raising service costs (air conditioning, water desalination) and impacting food security, reducing people’s ability to access healthcare.28
Coping strategies: mitigation and resilience approaches
Thomson et al13 propose a maturity matrix to assess resilience against climate change. Their model highlights two key approaches: adaptation (reducing negative impacts) and mitigation (reducing greenhouse gases). While climate risks are unavoidable, their effects on health systems and economies can be lessened through a combination of mitigation and adaptation strategies. However, effective interventions require thorough assessments of climate challenges on health systems. Climate risk management plays a crucial role in designing and implementing climate programs. This involves assessing risks, developing solutions, and adapting to changing conditions. It considers vulnerability assessments, government policies, and projected health and environmental impacts. Historical data is also vital to monitor progress. Risk assessments should be the first step in any management plan and continuously reviewed throughout the process.
Promoting adaptation and resilience
Adaptation to climate change involves adjusting existing systems (e.g., early warning systems, flexible policies) to minimize impacts and maintain progress towards development goals.29 Predicting the health consequences of climate change, such as increased treatment costs and unequal healthcare access, is crucial for understanding the ethical and legal implications, especially for vulnerable populations. This knowledge can inform strategies to improve population resilience. A resilient health system can predict, respond to, and adapt to climate shocks while maintaining service delivery.30 This requires a well-trained health workforce equipped to identify, prevent, and manage climate-related health risks.30 Community resilience, the ability to thrive in the face of change, is built through community-based planning processes where residents define solutions to their specific vulnerabilities.31,32
Social capital boosts community resilience
Strong social connections (social capital) are crucial for building community resilience to climate change.33 Examples include sharing cultural values and resources after disasters, or educational campaigns that promote environmental protection measures.34 Social capitals also help communities adapt by facilitating information sharing and access to support during crises. However, political divisions can hinder these efforts. Public education promoting coping mechanisms can help overcome these obstacles. Importantly, adaptation strategies must be tailored to each region’s specific vulnerabilities.13
Mitigation strategies: reducing greenhouse gas emissions
The healthcare sector is a major contributor to greenhouse gases, responsible for 4.4% globally.20 These emissions harm public health through air pollution and climate change impacts like heatwaves.22 Reducing emissions from healthcare improves air quality and reduces health risks, especially for vulnerable populations. Long-term benefits include moderating temperature extremes, improving crop production, and minimizing the spread of infectious diseases. Research gaps exist in understanding the relationships between CO2 emissions, health outcomes, and research & development efforts. Additionally, there’s a lack of coherent policies to reduce emissions and improve population health. Here are three main approaches to mitigating climate change:
Decarbonization, utilizing established technologies like renewable energy and carbon capture to reduce emissions, is one approach to tackling climate change. Negative Emission Technologies, which remove CO2 from the atmosphere through techniques like afforestation or direct air capture, offer another solution. Finally, Radiative Geoengineering, which explores theoretical techniques like stratospheric aerosol injection to manage solar radiation and potentially cool the planet, presents a more speculative approach.35 These techniques are still in early stages and carry significant risks. Finally, genetically modified crops with reduced water consumption and methane emissions offer another potential mitigation strategy, particularly for local impacts.
Discussion
Climate change, a result of human activities, is a recognized reality with direct and indirect impacts on public health. Risks include heatwaves, storms, floods, fires, changes in infectious disease patterns, impact on food yields, freshwater resources, ecosystem disruption, and displacement of vulnerable populations. Decisions made in the next few decades will determine the future climate and sea level changes.22 Indirect effects of climate change on basic human needs such as food, water, and shelter will likely have the greatest global health impact.36 By the end of the century, a significant portion of the world’s population will probably face severe food shortages and water insecurity. The health of millions is at risk through increased frequency of severe storms causing flooding and direct damage, leading to unemployment, homelessness, displacement, migration, and conflict. These can significantly increase stress, anxiety, and depression, disrupting mental and physical health. Many emerging impacts of climate change on public health are due to existing economic, social, and health inequalities.35 Inequalities in these “social determinants” of health will likely create inequalities in the capacity to adapt to climate changes.37,38 Given the climate emergency, urgent development of mitigation and adaptation mechanisms is crucial. Two main strategies for climate change are mitigation and adaptation. Uncertainty in future climate conditions challenges decision-making and development of these activities.38 Sectors like water infrastructures, land use planning, building and housing infrastructures, and transportation should consider climate changes in adaptation strategies. The health sector, often overlooked, is responsible for various adaptation activities and is a key partner for health-related activities. There’s no final solution to climate change; all sustainable technologies and techniques should be used. Radiative geoengineering is interesting but not a long-term solution as it does not address the root cause. Technologies need to be developed, tested, and side effects considered, which may take time.
Conclusion
Climate change’s impact on global health is reaching catastrophic levels, with no country immune. Millions are at risk of disease outbreaks, heatwaves, water and food shortages, air pollution, and poverty. Basic health systems provide resilience, offering accessible, cost-effective, responsive care. It’s time to build climate-resilient health systems, using adaptation, resilience, and mitigation approaches to enhance capacity, manage risks, strengthen collaboration, and plan actions. Addressing current gaps and improving performance isn’t enough to prepare for climate change’s effects. Health systems must understand how climate changes affect their ability to manage health, evaluate intervention effectiveness under diverse conditions, and increase capacities. Therefore, it is necessary to evaluate the health system’s conditions, capacity, function, and capability before any action, to identify weaknesses and strengths and plan appropriate strategies.
Competing Interests
The authors have no conflict of interest to report.
Ethical Approval
Not applicable.
Funding
This research received no external funding.
References
- Hickmann T, Widerberg O, Lederer M, Pattberg P. The United Nations Framework Convention on Climate Change Secretariat as an orchestrator in global climate policymaking. Int Rev Adm Sci 2021; 87(1):21-38. doi: 10.1177/0020852319840425 [Crossref] [ Google Scholar]
- Shukla AR, Skea J, Reisinger A, Slade R, Fradera R, Pathak M, et al. Summary for Policymakers. Cambridge, UK: Cambridge University Press; 2022.
- Mock CN, Smith KR, Kobusingye O, Nugent R, Abdalla S, Ahuja RB, et al. Injury Prevention and Environmental Health: Key Messages from Disease Control Priorities. Washington, DC: The International Bank for Reconstruction and Development, The World Bank; 2018.
- Mosadeghrad AM, Isfahani P, Eslambolchi L, Zahmatkesh M, Afshari M. Strategies to strengthen a climate-resilient health system: a scoping review. Global Health 2023; 19(1):62. doi: 10.1186/s12992-023-00965-2 [Crossref] [ Google Scholar]
- Morfeld P, Erren TC. Countdown on health and climate change: too important for methodological errors. Lancet 2021; 398(10294):26. doi: 10.1016/s0140-6736(21)00884-9 [Crossref] [ Google Scholar]
- Raffa RB, Eltoukhy NS, Raffa KF. Implications of climate change (global warming) for the healthcare system. J Clin Pharm Ther 2012; 37(5):502-4. doi: 10.1111/j.1365-2710.2012.01355.x [Crossref] [ Google Scholar]
- McMichael AJ, Friel S, Nyong A, Corvalan C. Global environmental change and health: impacts, inequalities, and the health sector. BMJ 2008; 336(7637):191-4. doi: 10.1136/bmj.39392.473727.AD [Crossref] [ Google Scholar]
- World Health Organization (WHO). Quantitative Risk Assessment of the Effects of Climate Change on Selected Causes of Death, 2030s and 2050s. WHO; 2014.
- World Health Organization (WHO). 2021 WHO Health and Climate Change Global Survey Report. WHO; 2021.
- Tidman R, Abela-Ridder B, de Castañeda RR. The impact of climate change on neglected tropical diseases: a systematic review. Trans R Soc Trop Med Hyg 2021; 115(2):147-68. doi: 10.1093/trstmh/traa192 [Crossref] [ Google Scholar]
- World Health Organization (WHO). WHO Guidance for Climate-Resilient and Environmentally Sustainable Health Care Facilities. WHO; 2020.
- Li A, Toll M, Bentley R. Mapping social vulnerability indicators to understand the health impacts of climate change: a scoping review. Lancet Planet Health 2023; 7(11):e925-37. doi: 10.1016/s2542-5196(23)00216-4 [Crossref] [ Google Scholar]
- Thomson D, Varangu L, Webster RJ. A climate resilience maturity matrix for Canadian health systems. Healthc Manage Forum 2023; 36(4):217-23. doi: 10.1177/08404704231169037 [Crossref] [ Google Scholar]
- Somani R. Global warming in Pakistan and its impact on public health as viewed through a health equity lens. Int J Soc Determinants Health Health Serv 2023; 53(2):27551938231154467. doi: 10.1177/27551938231154467 [Crossref] [ Google Scholar]
- Conradt T, Engelhardt H, Menz C, Vicente-Serrano SM, Farizo BA, Peña-Angulo D. Cross-sectoral impacts of the 2018-2019 Central European drought and climate resilience in the German part of the Elbe River basin. Reg Environ Change 2023; 23(1):32. doi: 10.1007/s10113-023-02032-3 [Crossref] [ Google Scholar]
- Hartwell C, Lovell S, Hess JJ, Dolan K, Vickery J, Errett NA. Barriers and facilitators to state public health agency climate and health action: a qualitative assessment. BMC Public Health 2023; 23(1):145. doi: 10.1186/s12889-023-14996-2 [Crossref] [ Google Scholar]
- Riva M, Kingunza Makasi S, O’Sullivan KC, Das RR, Dufresne P, Kaiser D. Energy poverty: an overlooked determinant of health and climate resilience in Canada. Can J Public Health 2023; 114(3):422-31. doi: 10.17269/s41997-023-00741-0 [Crossref] [ Google Scholar]
- Scarr JP, Jagnoor J. Identifying strategic priorities for advancing global drowning prevention: a Delphi method. BMJ Glob Health 2023; 8(9):e013303. doi: 10.1136/bmjgh-2023-013303 [Crossref] [ Google Scholar]
- Kobayashi K, Wang X, Wang W. Genetically modified rice is associated with hunger, health, and climate resilience. Foods 2023; 12(14):2776. doi: 10.3390/foods12142776 [Crossref] [ Google Scholar]
- Fehrer V, Poß-Doering R, Weis A, Wensing M, Szecsenyi J, Litke N. Climate change mitigation: qualitative analysis of environmental impact-reducing strategies in German primary care. Eur J Gen Pract 2023; 29(1):2232946. doi: 10.1080/13814788.2023.2232946 [Crossref] [ Google Scholar]
- Rocklöv J, Semenza JC, Dasgupta S, Robinson EJ, Abd El Wahed A, Alcayna T. Decision-support tools to build climate resilience against emerging infectious diseases in Europe and beyond. Lancet Reg Health Eur 2023; 32:100701. doi: 10.1016/j.lanepe.2023.100701 [Crossref] [ Google Scholar]
- Omri A, Kahouli B, Afi H, Kahia M. Impact of environmental quality on health outcomes in Saudi Arabia: does research and development matter?. J Knowl Econ 2023; 14(4):4119-44. doi: 10.1007/s13132-022-01024-8 [Crossref] [ Google Scholar]
- Chen A, Murthy V. How health systems are meeting the challenge of climate change. Harv Bus Rev 2019;18.
- Hess J, Boodram LG, Paz S, Stewart Ibarra AM, Wasserheit JN, Lowe R. Strengthening the global response to climate change and infectious disease threats. BMJ 2020; 371:m3081. doi: 10.1136/bmj.m3081 [Crossref] [ Google Scholar]
- Heaviside C, Macintyre H, Vardoulakis S. The urban heat island: implications for health in a changing environment. Curr Environ Health Rep 2017; 4(3):296-305. doi: 10.1007/s40572-017-0150-3 [Crossref] [ Google Scholar]
- Roos N, Kovats S, Hajat S, Filippi V, Chersich M, Luchters S. Maternal and newborn health risks of climate change: a call for awareness and global action. Acta Obstet Gynecol Scand 2021; 100(4):566-70. doi: 10.1111/aogs.14124 [Crossref] [ Google Scholar]
- Frontera A, Cianfanelli L, Vlachos K, Landoni G, Cremona G. Severe air pollution links to higher mortality in COVID-19 patients: the “double-hit” hypothesis. J Infect 2020; 81(2):255-9. doi: 10.1016/j.jinf.2020.05.031 [Crossref] [ Google Scholar]
- Ebi KL, Bowen K. Extreme events as sources of health vulnerability: drought as an example. Weather Clim Extrem 2016; 11:95-102. doi: 10.1016/j.wace.2015.10.001 [Crossref] [ Google Scholar]
- Magis K. Community resilience: an indicator of social sustainability. Soc Nat Resour 2010; 23(5):401-16. doi: 10.1080/08941920903305674 [Crossref] [ Google Scholar]
- Tong S, Confalonieri U, Ebi K, Olsen J. Managing and mitigating the health risks of climate change: calling for evidence-informed policy and action. Environ Health Perspect 2016; 124(10):A176-9. doi: 10.1289/ehp555 [Crossref] [ Google Scholar]
- White-Newsome JL. A policy approach toward climate justice. Black Scholar 2016; 46(3):12-26. doi: 10.1080/00064246.2016.1188353 [Crossref] [ Google Scholar]
- Schrock G, Bassett EM, Green J. Pursuing equity and justice in a changing climate: assessing equity in local climate and sustainability plans in US cities. J Plan Educ Res 2015; 35(3):282-95. doi: 10.1177/0739456x15580022 [Crossref] [ Google Scholar]
- Banks LH, Davenport LA, Hayes MH, McArthur MA, Toro SN, King CE. Disaster impact on impoverished area of US: an inter-professional mixed method study. Prehosp Disaster Med 2016; 31(6):583-92. doi: 10.1017/s1049023x1600090x [Crossref] [ Google Scholar]
- Burger J, Gochfeld M. Perceptions of severe storms, climate change, ecological structures and resiliency three years post-hurricane Sandy in New Jersey. Urban Ecosyst 2017; 20(6):1261-75. doi: 10.1007/s11252-017-0678-x [Crossref] [ Google Scholar]
- Fawzy S, Osman AI, Doran J, Rooney DW. Strategies for mitigation of climate change: a review. Environ Chem Lett 2020; 18(6):2069-94. doi: 10.1007/s10311-020-01059-w [Crossref] [ Google Scholar]
- Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet 2009; 373(9676):1693-733. doi: 10.1016/s0140-6736(09)60935-1 [Crossref] [ Google Scholar]
- Friel S, Marmot M, McMichael AJ, Kjellstrom T, Vågerö D. Global health equity and climate stabilisation: a common agenda. Lancet 2008; 372(9650):1677-83. doi: 10.1016/s0140-6736(08)61692-x [Crossref] [ Google Scholar]
- Bowen KJ, Friel S. Climate change adaptation: where does global health fit in the agenda?. Global Health 2012; 8:10. doi: 10.1186/1744-8603-8-10 [Crossref] [ Google Scholar]